The Baby-Friendly Hospital Initiative
The Baby-Friendly Hospital Initiative (BFHI) is a structured, comprehensive, quality improvement strategy by the World Health Organization (WHO) and United Nations Children’s Fund (UNICEF) geared towards improving maternity care practices with the aim of creating an optimal environment, protected from commercial influences, and is supportive of a family’s informed infant feeding goals. It has been implemented in thousands of hospitals and maternity care facilities around the world. It is based on the Ten Steps to Successful Breastfeeding and standards outlined in the Implementation Guidance: Protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services: the revised Baby-Friendly Hospital Initiative. While the BFHI is based on the Ten Steps, there is a significant difference between the two that is important to know. Click here to read about the difference between the Ten Steps and the BFHI.

Restoring Choice for Families
THE BABY-FRIENDLY HOSPITAL INITIATIVE SUPPORTS INFORMED INFANT FEEDING DECISIONS
“The first few hours and days of a newborn’s life are a critical window for establishing lactation and providing mothers with the support they need to breastfeed successfully.” WHO/UNICEF 2018
Years of commercial interests that supported care practices that interfered with the establishment of breastfeeding eliminated breastfeeding as a choice for many families around the world. The Baby-Friendly Hospital Initiative implements care practices that restores their choice to breastfeed and empowers families to make informed infant feeding decisions

The Ten Steps to Successful Breastfeeding
Step 1A
Comply fully with the International Code of Marketing of Breast-milk Substitutes and relevant World Health Assembly resolutions.
STEP 1A:
RATIONALE: Families need commercial free, objective information, as they make infant feeding decisions. Health professionals’ judgement must NOT be influenced by commercial pressures. (WHO/UNICEF 2018 P. 12)
Step 1B
Have a written infant feeding policy that is routinely communicated to staff and parents.
Step 1B
RATIONALE: Written policies are a means for ensuring the consistency of care and the sustainability of evidenced-based practices. Policies create a mechanism for accountability and equity in care. (WHO/UNICEF 2018 P. 13)
Step 1C
Establish ongoing monitoring and data-management systems.
Step 1C
RATIONALE: Monitoring compliance with the infant feeding policy enables facilities to identify opportunities for additional staff training and quality improvement activities. (WHO/UNICEF 2018 P. 13)
Step 2
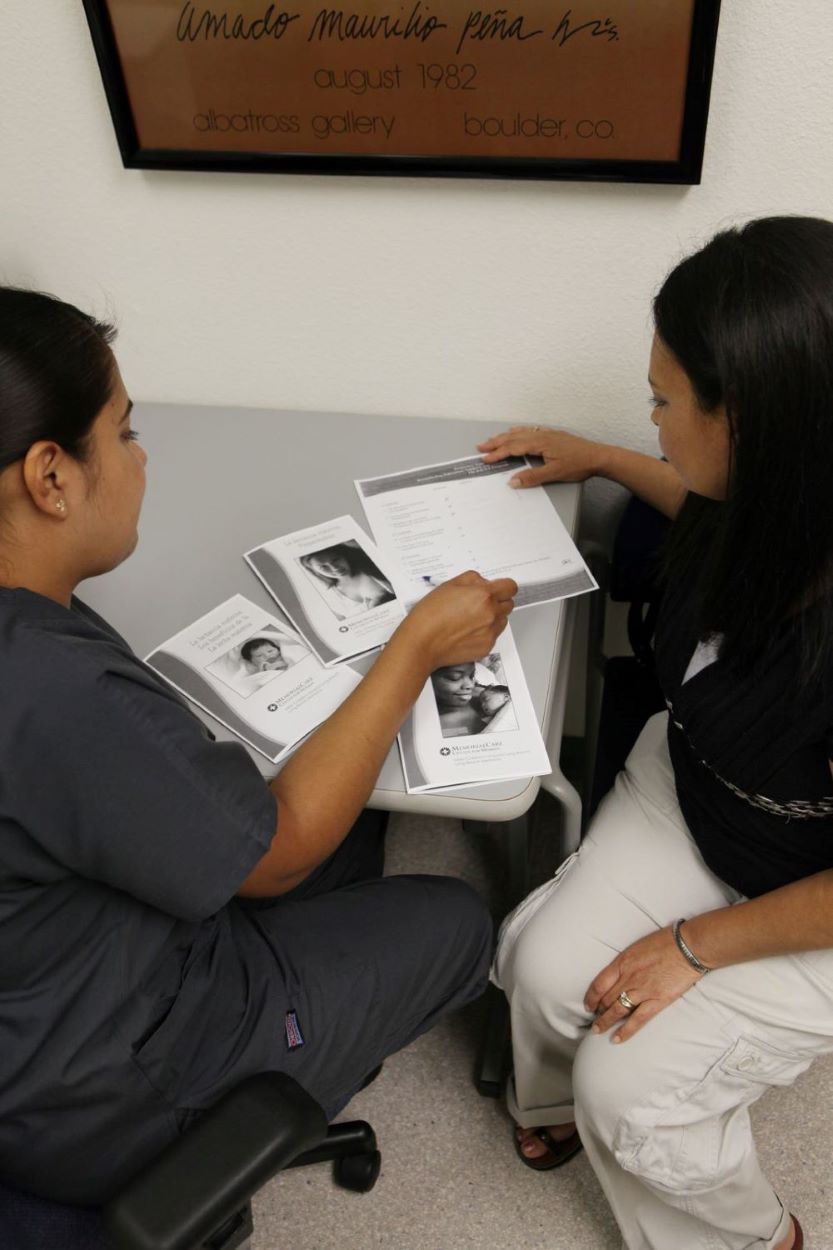
Ensure that staff have sufficient knowledge, competence and skills to support breastfeeding.
Step 2
RATIONALE: Competency verification is an important tool for ensuring all direct care providers have the appropriate knowledge, skills and attitudes necessary to deliver evidence-based, compassionate care. (WHO/UNICEF 2018 P. 14)
Step 3
Discuss the importance and management of breastfeeding with pregnant women and their families.
Step 3
RATIONALE: Pregnancy is an essential time for providing families with evidenced-based information about optimal infant feeding and care practices that support breastfeeding and bonding. (WHO/UNICEF 2018 P. 15)
Step 4
Facilitate immediate and uninterrupted skin-to-skin contact and support mothers to initiate breastfeeding as soon as possible after birth.
Step 4
RATIONALE: Immediate and uninterrupted skin-to-skin care helps stabilize the mother and infant post birth. It enables early breastfeeding which is associated with reduced infant mortality. (WHO/UNICEF 2018 P. 17)
Step 5
Support mothers to initiate and maintain breastfeeding and manage common difficulties.
Step 5
RATIONALE: Breastfeeding is a learned skill between mother and infant. Skilled lactation support in the early hours and days can help build maternal confidence and prevent future problems. (WHO/UNICEF 2018 P. 18)
Step 6
Do not provide breastfed newborns any food or fluids other than breast milk, unless medically indicated.
Step 6
RATIONALE: Exclusive breastfeeding is the best and healthiest option for mothers and babies without specific health programs or needs. It is the best way to establish a good milk supply. (WHO/UNICEF 2018 P. 19)
Step 7
Enable mothers and their infants to remain together and to practise rooming-in 24 hours a day.
Step 7
RATIONALE: Rooming-in enables mothers and families to learn their infant’s cues for feeding and other needs. This supports breastfeeding and the development of caring and nurturing relationships. (WHO/UNICEF 2018 P. 20)
Step 8
Support mothers to recognize and respond to their infants’ cues for feeding.
Step 8
RATIONALE: Responsive feeding is critical to building up an adequate milk supply and supports establishing a caring and nurturing relationship with the baby. (WHO/UNICEF 2018 P. 21)
Step 9
Counsel mothers on the use and risks of feeding bottles, teats and pacifiers.
Step 9
RATIONALE: Artificial nipples pose many risks to breastfeeding. Parents should be fully informed as they make decisions regarding their use. (WHO/UNICEF 2018 P. 21)
Step 10
Coordinate discharge so that parents and their infants have timely access to ongoing support and care.
Step 10
RATIONALE: Families learn basic breastfeeding skills during the hospital stay but may encounter challenging situations post discharge. Ongoing support is essential to help them achieve their goals. (WHO/UNICEF 2018 P. 22)
Supporting Families Through Competent, Compassionate, Care